We all enjoy a glass of wine or a cold beer every now and then…some of us more so. How does the weight gain, the hangovers, the lack or increase in appetite, mood swings and long term health problems relate to a night out?
I thought I would have a bit of fun and map out at least part of the biochemical processes that occur to understand how alcohol may affect our bodies.
I believe that if people understood the role of alcohol in their biochemistry they may think twice about drinking too much, but also understand how this may impact on their health conditions.
However, this is an information intensive article, so if you are not familiar with mitochondrial function and redox molecules I would suggest that you read the following articles first:
Mitochondrial Dysfunction – What Does It Mean For You?
Mitochondria – NADH and ATP Production via Different Pathways.
Normal Glycolysis pathway
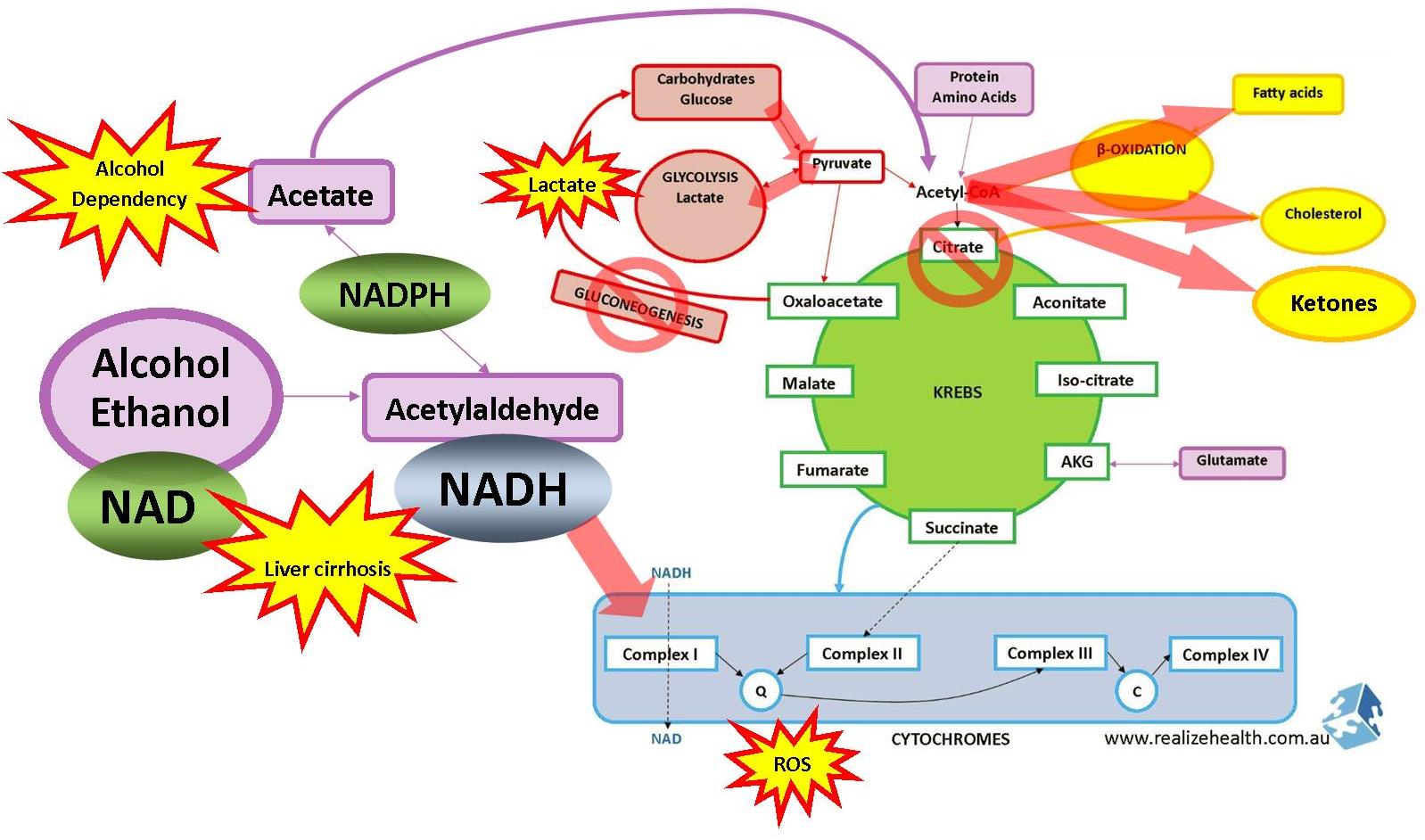
This is the normal pathway of glucose/sugar metabolism where food turns to glucose, glucose triggers an insulin response, insulin activates the GLUT transporters on the cell membranes, glucose enters muscle and fat cells, turns into pyruvate, then acetyl-CoA that enters the krebs cycle and produce NADH. NADH is further converted into energy/ATP during step-by-step processes in the mitochondria. This is how your body produces energy from food. Keep in mind that this cycle occurs in every single cell of our body (exception being red blood cells) so the liver is very much included here.
You can also read more about energy production through the different pathways and their efficiency in the article Mitochondria – NADH and ATP Production via Different Pathways.
Apart from the fact that alcohol/ethanol uses up valuable resources and antioxidants that would inevitably put a strain on methylation and other biochemical and liver pathways, what else happens when we drink alcohol?

Stage 1 – Dinner and Drinks!
You go out with some friends in the city, have some dinner and a few drinks. Alcohol is metabolized a lot faster than the slow process of digestion that food has to go through, so it has a head start on food as a fuel.
Alcohol can be broken down via 3 different biochemical pathways to produce acetylaldehyde (a toxic byproduct responsible for hangover symptoms). Acetylaldehyde is further broken down by ALDH (Aldehyde Dehydrogenase) into acetate. Acetate is harmless and produces no symptoms. This is why some people can drink a lot without any noticeable effects whilst others can only tolerate a small amount of alcohol before they feel a bit tipsy. It all depends on those ALDH enzymes.
However, if the oxidative stress is too much it will inhibit ALDH and slow down the breakdown of acetylaldehyde. Oxidative stress can be anything from bad diet, infections or environmental toxicity. All of these things can affect how well you metabolize alcohol. A very common complaint I hear from chronically ill clients is ‘I used to be able to enjoy alcohol at social events, but since I got sick I just cannot drink any alcohol without being affected for days.’ This is because their cells are exposed to a large amount of oxidative stress at that point in time.
Acetylaldehyde can bind to dopamine (a neurotransmitter that gives us joy and motivation) contributing to mood disorders commonly seen with drinking such as depression or aggression, and give you a worse hangover that will last longer.


Consuming alcohol uses up a lot of NAD (vitamin B3) in the process and produces NADH, and remember that NADH is a high energy molecule which you can read about in the article Mitochondria – NADH and ATP Production via Different Pathways. So, now you have all this NADH being produced by alcohol metabolism and not by the citric acid cycle.
It can enter the cytochrome pathway (ETC) directly where NADH is the first step in complex 1. This will speed up ETC, produce more energy but also more free radicals in the process and put increased demand on Coenzyme Q10, vitamin B2 (riboflavin) and iron.
Why Taking B Vitamins Before You Go Out and the Next Morning Helps
Back to our story.
Alcohol as mentioned had a headstart in NADH production and NADH is a high energy molecule. So you feel great! You feel energized, happy and animated. Life is good. You finished your meal and now it’s off to the clubs, either to drink some more or maybe dance. Your food starts to digest and release more glucose into the cells. Ready to be burned for energy.


Food moves from the stomach to the small intestine 1-2 hours after eating. This is where final digestion of carbohydrates take place using disaccharidase enzymes present on the villi lining the small intestinal wall. Disaccharides (complex sugars from carbohydrates) are broken down into monosaccharides (simple sugars from carbohydrates) or glucose, gets absorbed into the bloodstream by pulling sodium with it and potassium out of the blood and into the cells via GLUT (glucose transporter) receptors.
This means that alcohol is the preferred form of energy production up until 2 hours after eating.
Why electrolytes are so important
But wait!
The electron transport chain (ETC or cytochrome chain) already has plenty of NADH to deal with (depending on how much you are drinking off course) and doesn’t want anymore food / electrons / NADH. So, it down-regulates energy production and slows down the krebs cycle inside the mitochondria.
Here is where our story forks into two roads. The road you choose will have different outcomes.
Stage 2a – I’m Not a Good Dancer
You don’t like to dance or you think you look silly. So you choose to sit at the bar, chat and have a few more drinks. This just adds more energy-loaded NADH molecules with nothing to do. They start to clogg up your cytochrome chain (you really need some CoQ10 here) and glucose that is not entering the krebs cycle is being shunted to glycolysis instead. It will go around-and-around producing lots of lactate in the process.
Lactate can make you feel very tired, lethargic and experience muscle pains or fatigue (fibromyalgia).
This means metabolism is shifting away from oxidative phosphorylation (inside the mitochondria) that requires oxygen towards anaerobic metabolism that does not require oxygen. This could also be a mechanism the body uses to protect itself against more free radical damage by not going down the krebs cycle or ETC and just remaining in glycolysis, recirculating pyruvate over and over again.
A lot of lactate is produced during anaerobic metabolism which contributes to acidity and increased demand for nutrients such as creatine and magnesium.
Creatine is produced from methylation so again we see increased strain on the methylation cycle.
Magnesium is an important mineral involved in blood sugar control, leptin resistance and other weight gain hormones.
Why you wake up in the morning feeling like you got run over by a bus

The body can also get rid of this accumulated glucose via other (more unfavourable) pathways which produce a lot of free radicals (ROS) in the process. This increases the demand for antioxidants such as glutathione which will put further strain on the mitochondria and methylation cycle.
These pathways are:
- Polyol pathway
- Hexosamine pathway
- Methylglyoxal pathway
- Dihydroxyacetone pathway
- Alpha-ketoaldehyde pathway
All of these roads lead to chronic disease.
NADH (being high energy) will also send the signal to your brain that you don’t need any more fuel. You have too much already. So you may not feel that hungry. Sure, if you are in fact eating, it may be more out of habit. The bowl full of peanuts is sitting right there and as your brain is fueled on acetate you’re not really that aware of what you are doing. So you just pick at it out of….boredom?
Not generally out of hunger.
Following a cascade of reactions after ATP production you get vagal nerve stimulation that signals to the brain that you are full and don’t need to consume any more food or fuel for energy production. This is often why people who consume a lot of alcohol forget to eat or don’t feel hungry.
Stage 2b – I Love To Dance
OK, so you don’t mind looking silly, have lots of confidence and just love to dance. It’s a good thing too because you have all this NADH energy molecules looking for some action. Might as well take them out for a dance.
I’ll make a small confession here, not to brag but to illustrate a point. I’ve always been a competitive athlete since high school and in recent years have even been teased by the lure of semi-professional competition. Running half-marathons at 3:45 minutes per kilometer (apologies to those who don’t follow the metric system) put me in a very good running category (1 hour 20 min) but just shy from being really amazing. At the height of my fitness (would have easily been doing 3 hours of training per day and was as skinny as a rake) I remember going out to my now-sister-in-law’s bachelorette party and having a really good time (not excessive because very fit people don’t handle their alcohol too well – a good article for another time) as you would. By 3am everyone crashed into bed but I was as energetic as anything (even after dancing the whole night).

So, I did the next best thing.
Went for a run at 3am along the beach…it wasn’t even a run, more like a sprint. I ran 10km in 34 minutes, and the next day had no hangover whatsoever. If I could describe it I felt like I was running on ethanol fumes. And as soon as I burned that all off I felt really good. Certainly not something I would recommend to anyone, but an interesting observation.
I don’t have science to back this up, but from personal experience combined with what I know now, I would interpret it as follows:
When you are very fit or have excellent mitochondrial function, the tendency would be to want to burn off the excess NADH instead of slowing the krebs cycle down. So your body sends you signals to be more active to try and get rid of this excess energy. Athletes also have lots more mitochondria than the average person, so more workers available to get rid of NADH. If you are healthy and have all the cofactors available for the cytochrome chain (B2, B3, CoQ10, healthy thyroid) you can turn excess NADH into energy in no time.
This poses the question whether those who start feeling very lethargic on alcohol quickly have very poor mitochondrial health or lack the cofactors for healthy ETC function.
Maybe you want to have your thyroid checked (please, not just TSH as this is not even a thyroid hormone) if you feel super tired every time you drink alcohol (within reason off course).
It also illustrates the point that excess NADH (if it’s not burned off) is contributing to the hangover you get the next day.
How?
If NADH is inhibiting krebs cycle enzymes, then acetyl CoA cannot enter the krebs cycle. Acetate will start to build up (if the liver is struggling to clear it all) and slow down metabolism of acetylaldehyde into acetate. So both acetylaldehyde and acetate will start to accumulate, responsible for hangover symptoms.
Another important reason why liver support helps with hangovers.
Important reason why physical activity is important around alcohol consumption.
Stage 3a – I Think I May Be In Trouble
What happens when there is too much glucose and NADH (ie too much food and alcohol) to be burned for energy? It will be stored as glycogen or fat. When the cells are filled with glucose it will stop absorbing any more glucose and blood sugar levels will start to go up. Glucose is transported back to the liver to be stored as fat.
Blood sugar levels will then drop (because gluconeogenesis is inhibited) and will continue until you get cravings for hot chips and pizza at 3am in the morning. The low blood sugar you experience may cause mood swings and contribute to hangovers.

Why Having Starchy Food ‘Cures’ Your Hangover
Due to the increased NADH production from alcohol it starts to accumulate and the body doesn’t know what to do with it, or can’t process it fast enough. Because the mitochondria also produces NADH, the body will signal for the mitochondria too slow down because it doesn’t need any more NADH to be produced. This will also slow down energy/ATP production which would explain the fatigue that follows alcohol consumption. Also the puffiness (glycogen) and eventual weight gain.
Fat metabolism (through β-oxidation) also increases NADH, so your body will immediately stop the breakdown of anymore fats (until the need for NADH increases again). In fact, it could actually increase the production of more fats, leading to fatty liver. Excess glucose in the blood is transported back to the liver where it is converted into fatty acids and triglycerides. It is stored in the liver (fatty liver) or transported back into the blood as triglycerides (atherosclerosis).
Now if you keep on drinking alcohol will be metabolized via a 2nd pathway called MEOS (microsomal ethanol-oxidizing system). This pathway puts a real strain on your antioxidants which is already in trouble from all the excess NADH it is trying to process.
MEOS is a cytochrome P450-dependent pathway (CYP2E1) in the liver that breaks down alcohol into acetylaldehyde and then acetate using up valuable NADPH. NADPH is needed to regenerate glutathione. If NADPH is used up for alcohol metabolism, not enough is left over for glutathione regeneration which will affect antioxidant status and detoxification of other environmental toxins. Considering that a lot of ROS (free radicals) are produced during alcohol metabolism already and the liver is already under strain, you need all the antioxidants and glutathione you can get.
Why taking liver herbs helps you feel better
The acetate produced by MEOS is converted to acetyl CoA which would usually just enter the krebs cycle inside the mitochondria at the top to become citrate, but those pathways are blocked now (due to excess NADH from too much alcohol and/or food).
So where does acetyl CoA go?
Some of the acetyl CoA will convert to ketone bodies which will contribute to even more acidity as ketones are highly acidic (remember there’s already a lot of lactate floating around which makes you more acidic as well). When the liver can’t break down any more acetate, acetylaldehyde will start to accumulate instead creating brain fog and fatigue.

The acetylaldehyde also creates the flushing effect you get from drinking too much. Your face goes all red and the next morning you have a terrible headache. That is acetylaldehyde.
Acetylaldehyde is toxic stuff and is responsible for alcohol poisoning when drinking in excess.
Stage 3b – Maybe I’m OK?
If you managed to burn off all the excess NADH and you had good nutrition on your side – plenty of B vitamins and electrolytes – then you may be hangover free after all.
Stage 4 – Chronic Effects of Alcohol
Alcohol consumed at consistently high levels will damage the liver and lead to cell death. If this is a regular occurrence, liver damage will progress from fatty liver (as mentioned earlier) to alcoholic hepatitis to liver cirrhosis. Once the liver is damaged to this degree it loses its ability to remove ammonia via urea excretion. Ammonia is highly toxic to the nervous system and can lead to coma and death in extreme cases.
The liver will learn to upregulate the MEOS pathway if heavy drinking becomes a habit. The acetate produced fuels the brain and releases more adenosine which has a sedative/relaxant effect.
When you try to change your lifestyle and you go from heavy drinking to nothing at all, the brain becomes deprived from its acetate and adenosine ‘hit’. It’s this lack of acetate that causes alcohol withdrawal symptoms.
Taking adenosine or drinking apple cider vinegar may help with withdrawal.
Prolonged exposure to too much acetate may cause liver and brain inflammation. Acetate increases blood flow to the liver and depresses the nervous system. Some of this acetate will be converted to acetyl CoA which will fuel cholesterol synthesis instead of energy production especially if the krebs cycle is slowed.
This Also Relates To Other Stuff
Even though this post is an exploration around alcohol, it could easily be duplicated for yeast infections or high carbohydrate diets / overeating. It follows roughly the same pathways and create similar biochemical blocks.
References:
Thanks to Dr. Ben Lynch for providing this alternative insight into glucose metabolism at SHEICON15