Atherosclerosis and heart disease is one of the biggest modern day killers in our society.
Part of the blame I believe sits with the outdated food pyramid that is still to this day being plugged as the ‘go to’ for dietary recommendations. You will notice that the people who are the leanest and healthiest in society do NOT eat according to the food pyramid, so I rest my case.
But there are also some biochemical aspects to cardiovascular disease that I think is pretty interesting and worthwhile looking at, since atherosclerosis like all other ‘diseases’ are disorders of cellular function.
OUR FAT TRANSPORTERS
Carnitine is the methylated end-product of the essential amino acids lysine and methionine, and phosphatidylcholine is the methylated end-product of choline.
Both these nutrients have a role in preventing cardiovascular disease. These are both surrounded with some controversy where they can be both beneficial and detrimental depending on nutritional status, genetic polymorphisms and the gut microbiome of the person. And of course which studies you choose to read.
Because these are nutrients I use a lot in my practice I decided to investigate it a bit further whilst also looking at other factors in atherosclerosis.
TMA AND TMAO – RELATIONSHIP WITH CHOLINE AND CARNITINE
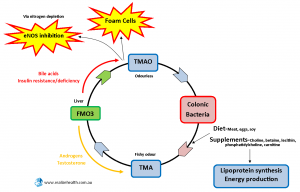
Choline (found in eggs, lecithin, phosphatidylcholine, phosphatidylethanolamine) ensures the structural integrity of cell membranes, cell signalling and act as a methyl donor. Choline is needed for lipoprotein synthesis which carries cholesterol away from the blood vessel walls, and deficiency has been associated with fatty liver, liver damage and DNA damage.
Metabolic Syndrome and Fatty Liver
Carnitine transports fatty acids into the mitochondrial matrix for energy production and has good anecdotal evidence for lowering triglyceride levels in the blood.
Our diets determine the species of gut flora we harbor in our digestive systems. Eating high meat diets will tend to favor higher counts of Acinetobacter and Prevotella in the large intestine, and these bacteria are responsible for converting carnitine and choline to TMAO.
TMAO (trimethylamine N-oxide) is an odourless amine oxide that is oxidized into TMA (trimethylamine) which is derived from choline. TMA will move from the digestive tract into the bloodstream but typically does not cross the cell membranes into the cells. This is only likely to occur where cell membranes are damaged due to high homocysteine/AGEs or cell membrane break down related to choline deficiency or upregulation of phospholipases. I am highlighting this because it is a common occurrence in those with chronic illnesses that are difficult to resolve.
So when tight junctions in cell membranes are damaged in the gut, TMA will move from the gut to circulation, be converted into TMAO and move back from circulation to the gut. This could explain the delay in seeing increased TMAO levels after ingesting meat or choline-rich foods. TMAO movement back into the digestive tract could also serve as a substrate for anaerobic metabolism by gut bacteria where it is reduced to TMA.
When TMA is not metabolized back into TMAO or allowed to accumulate, you develop a fish odour in sweat, urine and breath after consuming foods or supplements high in choline or carnitine. According to research high TMAO has been associated with atherosclerotic lesions by promoting cholesterol accumulation within macrophages and subsequent foam cell formation.
So, this is important…
If you develop a fish odour smell when you take carnitine supplements it may indicate gut dysbiosis, leaky gut and leaky cell membranes.
You can read more about this in our eBook ‘Leaky Gut, Leaky Cells, Leaky Brain…’
Fish apparently contains higher amounts of TMAO than red meat. After eating the fish some of the TMAO is used but most of it is reduced back to TMA by gut organisms as explained above.
SO, DOES THIS MEAN MEAT IS BAD?
I don’t think so.
Chris Masterjohn’s response to the research done on this subject makes more sense to me.
I believe there is a bigger gut microbial involvement here due to the fact that vegans and meat eaters responded differently to the same meals and supplements with regards to TMAO levels. Leaky gut would also play a big role as already mentioned.
FMO3 (FLAVIN MONO-OXYGENASE 3)
As the name suggests it is dependent on riboflavin or Vitamin B2 for its function as well as iron. It is down-regulated by androgens (low TMAO) and upregulated by dietary bile acids, diabetes and metabolic syndrome (high TMAO). We can conclude from this that low testosterone may contribute to atherosclerosis through the up-regulation of the FMO3 gene. This may explain testosterone’s protective function and why men, either through the natural drop in testosterone levels as they age or increased aromatization of testosterone, are more at risk of developing atherosclerosis.
Also remember that Vitamin B2 is implicated in MTHFR C667T polymorphisms and thyroid function. Similarly the thyroid hormone, T4 or thyroxine, is necessary for riboflavin’s conversion to the active redox molecule FAD.
LDLR (LOW DENSITY LIPOPROTEIN RECEPTORS)
When these receptors are missing or down-regulated due to the lack of estrogen in women, such as during menopause, and more fat is consumed, less betaine and DMG is excreted in the urine and the same metabolic changes associated with ApoE gene defects are observed.
This is very important. For post-menopausal women LDLR gene expression is likely a lot more common than ApoE gene gene expression.
Conversely when LDLR is upregulated or overexpressed it seems to increase the clearance of amyloid beta in the brain which holds great promise for Alzheimer’s disease. In the periphery LDLR removes cholesterol from the circulation and may be upregulated with green tea catechins, mulberry extract and goldenseal (presumably through berberine content).
HOMOCYSTEINE
Although SAH (S-adenosylhomocysteine) is a more reliable marker for atherosclerosis risk and methylation imbalances, it is expensive to test for and most people are more familiar with homocysteine, so we’ll use this marker for discussion instead.
Vitamin B12 (cobalamin), B2 (riboflavin), folate, choline and TMG (Trimethylglycine) all assist in the recycling of homocysteine, while vitamin B6 (pyridoxine-5-phosphate) and cysteine remove it through the CBS (Cystathionine beta-synthase) pathway to form glutathione, alpha keto-glutarate (AKG), hydrogen sulfide (H2S) or ammonia (NH4).
Glutathione regulates the methylglyoxyl pathway and prevents the formation of AGE’s associated with atherosclerosis.
When Vitamin B12 and folate levels run low the body will use choline to keep homocysteine recycling going. In the absence of dietary choline (ie vegans) the body will upregulate phospholipases to break down cell membranes and source choline from there.
This certainly is not the ideal situation.
NITROGEN
Nitrogen is a component of amino acids, abundantly found in green leafy vegetables, and needed for nitric oxide synthesis in the NOS (Nitric Oxide Synthase) cycle. Every time TMA is converted to TMAO through the FMO3 enzyme nitrogen is depleted which in the long run could inhibit NOS (Nitric Oxide Synthase).
NO (NITRIC OXIDE)
Nitric Oxide is a signalling ‘messenger’ that influences physiological processes and maintains homeostasis. Its main function is through the relaxation of vascular walls and improving circulation (eNOS), but it also has immune modulating effects (iNOS) and can also act directly as a neurotransmitter (nNOS).
Apart from its role in the cardiovascular system it also is involved in the development of the auditory system and other sensory systems. This brings up interesting thoughts around auditory and sensory integration issues often seen in children with autism or Asperger’s.
ADMA (ASYMMETRIC DIMETHYLARGININE)
When proteins are modified in cells during methylation they produce this metabolic byproduct. Its production is triggered by oxidized LDL cholesterol and it looks very similar to arginine.
The problem with ADMA is that it inhibits Nitric Oxide production (maybe due to competition with arginine to binding sites) which may lead to vasoconstriction and increases in blood pressure. High ADMA levels are often found with high blood pressure, oxidized LDL cholesterol, Diabetes mellitus and metabolic syndrome.
Balance this with the amino acids arginine, citrulline, ornithine and TMG.
A WORD ON STATINS
Statins inhibit the enzyme HMG-CoA reductase involved in cholesterol synthesis. This is how it lowers cholesterol levels and give you a ‘satisfactory’ number on your blood test result implying that you are doing something healthy for your heart.
Unfortunately this is also the same pathway needed for Co Q10 and isoprenylated protein synthesis, both of which are extremely important for healthy heart function and to stop the progression of atherosclerosis.
So while the numbers on your blood tests may satisfy your doctor, the deterioration continues. An interesting study done by Okuyama H. et al. (2015) in fact showed that statins worsened atherosclerosis over time and contributed to heart failure.
SO, WHAT DOES THIS MEAN?
It is interesting to see how nutritional deficiencies, hormone imbalances, metabolic syndrome and methylation dysregulation contribute to heart disease, to just name a few. It’s the combination of these that increases the risk for disease.
Do we stop eating protein or taking carnitine and choline supplements? No.
As usual it depends on case history, symptoms, genetic polymorphisms, diet and lifestyle.
The usual still applies.
Eat good quality protein (amino acids, taurine, choline, carntine), plenty of green leafy vegetables (nitrogen, folate), exercise (upregulates LDLR and improves cholesterol markers), listen to music and meditate (increases NO production), reduce processed carbs and sugars (improves insulin resistance and reduces TMAO formation).
With each discussion the processes and pathways we look at may change, but the treatments remain largely the same.