WHAT ARE OXALATES?
Oxalates and oxalic acids are organic acids that are produced from food metabolism, that can be measured in an Organic Acid Test (OAT). These play a part in mitochondrial dysfunction, mineral deficiencies and gut dysbiosis, and can come from dietary sources, yeast or fungal infections, or cellular metabolism.
Oxalates can be the source of a lot of unexplained symptoms such as:
- Poor sleep
- Fibromyalgia
- Vulvar pain
- Joint aches and pains
- Fatigue
- Eye pain
- Bedwetting or incontinence
- Kidney stones (calcium oxalate)
- Gout (iron oxalate)
Oxalate crystals are not just confined to the kidneys but can also deposit in the joints, blood vessels, lungs, bones, nerve tissue, retina, thyroid and brain, where it can cause pain, inflammation and damage to surrounding tissues. This is called oxalosis.
Studies have shown very high levels of serum and urinary oxalates in some autistic children, and can affect the biochemistry through:
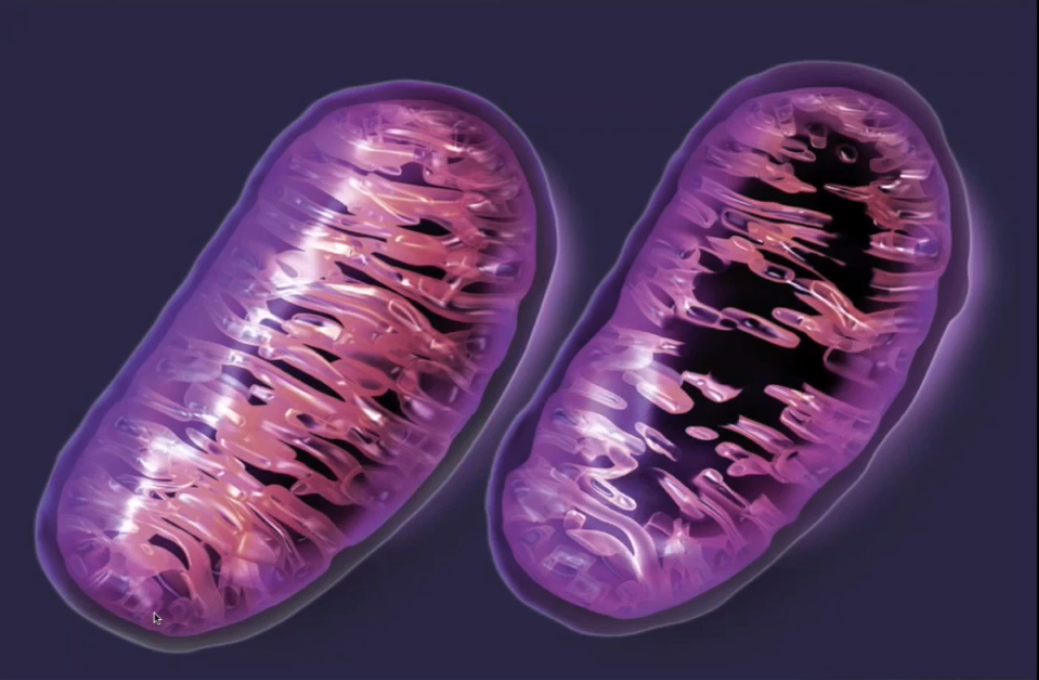
- Mitochondrial dysfunction
- Altered gene expression
- Altered cell membranes
- Increased ROS (reactive oxygen species) or free radicals
- PLA2 (phospholipase A2) activation
- Increased inflammation via cytokines, COX-2
DIET AND OXALATES
Dietary oxalates may compound already existing problems with oxalate breakdown due to gene mutations (hyperoxalurias), gut dysbiosis or nutritional deficiencies. It is beneficial to follow a low oxalate diet in the presence of high urinary oxalates to reduce symptoms and extra load on the body as oxalates drive salt complex or crystal formation. But you have to use this as a temporary measure whilst addressing the underlying biochemical or gut issues.
It is especially important to consider dietary sources when large amounts of green smoothies containing spinach, beetroot and other high oxalate vegetables are consumed on a regular basis, and even more so if these vegetables are not organic. A direct quote from Monsanto’s patent which can be accessed at the EPO website reads:
“[origin: WO02069718A2] Pesticidal concentrate and spray compositions are described which exhibit enhanced efficacy…
More particularly , the present invention relates to a method of enhancing the herbicidal effectiveness of glyphosate concentrate and tank mix formulations containing one or more surfactants through the addition of oxalic acid.”
Glyphosate is more commonly known as ’round-up’ and used as a herbicide in many gardens and farming practices. If you are consuming vegetables, grains or anything else that may have been grown using round-up, you may be adding to the oxalate load (amongst many other issues with glyphosates which will need a discussion on its own).
Some foods contain polyethylene glycol (PEG) which is a petroleum compound made from ethylene glycol (the main ingredient in anti-freeze) and is found commonly in sports drinks, laxatives, baked goods and creams.
Check out the Oxalate Food list.
FUNGI OR YEAST INFECTIONS
Candida organisms have been found surrounding oxalates stones in the kidney, and the presence of yeast infections have been correlated with high amounts of oxalates. Fungi can also produce vitamin C which may contribute to the next point below.
Certain probiotics seem to have a specific action around oxalate breakdown in the gut with lactobacillus acidophilus, lactobacillus plantarum, bifidobacterium lactis, bacteroides and oxalobacter formigenes mentioned. This could be another reason for oxalate accumulation in some and not others, where regular antibiotic use (either through prescription or food contamination) can disrupt the normal gut flora to such an extend that these species become deficient in some, leaving them less capable of dealing with even normal dietary loads of oxalates.
IS THERE A CONNECTION BETWEEN VITAMIN C AND OXALATES?
This only seems to be a factor when very high doses of supplemental Vitamin C is consumed in the presence of free copper in the blood. My thoughts on this is that high blood copper levels are often found with low zinc levels or high estrogen, so maybe high cadmium load in the body can contribute to zinc deficiency and possible increased conversion of vitamin C into oxalic acid.
Keynotes: Smoking
Human metabolism
OXALATE DUMPING
So once you get your test results back and it shows high levels of oxalates, the best course of action is to stop all oxalate foods, right?
Wrong…
If you pull oxalates too quickly from the diet you may create or experience ‘oxalate dumping’ which can make your symptoms worse. Remember that oxalates have a crystaline structure with sharp edges, and they look a little bit like glass-shards under the microscope. As these oxalata crsytals start to move out of the cells into the surrounding tissues, or from the tissues into the bloodstream, they irritate the surround tissues with their sharp structure. And oxalates will start to move if you eliminate too many oxalate-containing foods too quickly.
So be careful.
Typical signs of oxalate dumping include:
- Sandy or grainy stools
- Pain with urination
- Irritability, moodiness
- Toilet-training accidents in young children
- Painful bowel movements
- Rashes
- Yeast flare-ups
If this is a concern, remove oxalates very slowly from the diet at the rate of 5-10% per week. Cooking (boiling, roasting) vegetables can reduce oxalate content of vegetables by up to 50% but keep in mind that in very high oxalate foods even half the amount may still be very high. Oxalate dumping can continue for more than a year in some even after high oxalate sources have been removed. Drinking enough water and staying hydrated is very important.
OXALATES AND NUTRITIONAL DEFICIENCIES
Oxalates as a ligand will often bind to calcium, magnesium, iron and zinc in the intestines for elimination. This creates obvious nutritional deficiencies which has wide-range consequences for our biochemistry, hormones and neurotransmitters. Vitamin B6 deficiency in itself can contribute to oxalate problems.
Omega-6 is associated with increased oxalate problems and Omega-3 reduces them. This skews fatty acid ratio’s towards arachidonic acid which is more inflammatory and can contribute to depression.
If zinc absorption is diminished it may contribute to zinc:copper imbalances with higher levels of copper also associated with estrogen dominance. Lower levels of progesterone due to low zinc, B6 and magnesium may contribute to this problem. This may be one potential mechanism why estrogen dominance, high copper and yeast infections seem to coincide.
BILE AND FAT METABOLISM
Low bile salts with fat malabsorption and unabsorbed free fatty acids in the gut can bind to calcium during digestion to form insoluble ‘soaps’. This decreases calcium’s ability to bind to oxalates allowing more to be absorbed systemically. Bile salt production problems and sludgy bile consistency can often be linked back to methylation and trans-sulfuration imbalances as these pathways are necessary for taurine, choline and phosphatidylcholine production which are important components of bile.
Constipation is a consequence of low bile salt production and will create a gut environment favourable to even more yeast overgrowth (its role has already been discussed) which feeds into this viscous cycle.
METHYLATION AND OXALATES
Methylation nutrients such as vitamin B6 and B12, as well as Glutathione are needed for oxalate metabolism in the Citric Acid Cycle. This shows how poor methylation can be a contributing factor to oxalate build up in the cells, or how oxalates can disrupt methylation. Sometimes nutrients such as B6 do not bind very well to their receptors which can reduce the effectiveness of extra supplementation and will need to be addressed.
CBS dysregulation, either through genetic expression or environmental upregulation (such as yeast infections), can contribute greatly to oxalate formation due to its need for vitamin B6 and its role in the formation of bile salts and glutathione.
OXALATES AS CHELATORS
Oxalates in their dibasic anion form have a high affinity for binding with minerals and metals that are positively charged, such as calcium, magnesium, zinc, copper, lead, cadmium and mercury. These oxalate-mineral salt complexes have different solubility or Ksp values which is an indicator of how strong they are bonded together and how likely they are to disassociate and dissolve. Mercury-oxalate salts are about 100,000x less soluble than calcium-oxalate salts which makes them more likely to accumulate and get trapped in the tissues. This needs to be considered where dental amalgam fillings are being removed and when clearing oxalates. It may also be a good idea to not mix high oxalate and higher-risk metal foods in the same meal such as spinach and fish for example.
OXALATES AND GLYCOLYSIS
Oxalates inhibit PK (Pyruvate Kinase), the enzyme responsible for converting phosphoenolpyruvate to pyruvate. Pyruvate is produced as part of the glycolysis pathway in the breakdown of sugar to ATP/energy conversion. By blocking pyruvate formation it will stop glucose from being broken down to ATP in the krebs cycle. So you end up with low energy, glucose accumulation in the blood possibly further feeding yeasts, creating mood swings due to sugar imbalance, and forcing glucose through alternate pathways such as lactate or glycation.
OXALATES AND D-LACTATE
D-lactate produced by lactobacilli bacteria in the gut is metabolized by an enzyme called D-2-hydroxy acid dehydrogenase. High levels of oxalic acid inhibits this enzyme contributing to the build up of d-lactate in the gut. This lowers the gut pH further, encouraging more d-lactate production, and if these build up high enough, may affect mitochondrial function.
PYROLURIA
As an interesting side-note there seems to be a similarity between nutrients involved in pyroluria and oxalates – Vitamin B6, zinc, magnesium, biotin. My personal opinion is that most pyrolurias are not disorders on its own but rather part of a bigger picture. In this case it would be very plausible that mold/fungus/yeast issues are creating a deficiency in nutrients through oxalate binding that can then lead to secondary pyroluria.
CONSIDERATIONS
Testing for oxalates can be done through urinary Organic Acid Testing. There are some foods and nutrients that are very important for reducing oxalates, and others that can make it worse. It’s not always as simple as just following a low oxalate diet as these can be produced endogenously.
I regularly teach practitioners all over the world on the interpretation of the OAT (Organic Acid Test) used to measure oxalates having run full day workshops both in Melbourne Australia for GPL (Great Plains Laboratory), and London UK for Functional DX.
For more information on Oxalates, please read this very informative brochure from Great Plains Laboratories – Oxalates Control and find recipes and information on low oxalate diets from Dr. Susan Owens at Low Oxalate Diet or Julie Matthews at Nourishing Hope. Julie also wrote a really good article on the subject called Oxalates: Their Influence on Chronic Disease.
For some recipe ideas the following websites are really good:
http://lowoxalateinfo.com/
http://www.lowoxalate.info/recipes.html
http://mindd.org/s/uploads/pdf/LowOxalateSampleWeeklyMenu.pdf
References:
Oxalate toxicity in renal cells.
William Shaw, The Role of Oxalates in Autism and Chronic Disorders WAPF, March 26, 2010
J Konstantynowicz et al., European Journal of Paediatric Neurology 16(5), 2012, 485-491
https://data.epo.org/gpi/EP1389912A2-PESTICIDE-COMPOSITIONS-CONTAINING-OXALIC-ACID
Dempsey, et. al, Urinary Oxalate Excretion, Metab. Clilnic Exptl 9:52, 1960
Invest Urol. 1966 Sep;4(2):133-42. Calcium oxalate lithiasis produced by pyridoxine deficiency and inhibition with high magnesium diets. Lyon ES, et. al.
J Urol. 1982 Mar;127(3):598-604. Effects of magnesium deficiency on intratubular calcium oxalate formation and crystalluria in hyperoxaluric rats. Rushton HG, Spector M
Julie Matthews, Nourishing Hope
Image sourced from http://accurateclinic.com/accurate-education-mitochondrial-dysfunction/





are there doctors who you’ve trained in the western MA, USA, area, or surrounding area? Thank you so much for this info, which is the first time I’ve seen an explanation that brings my health issues & contributing factors together. I’m in serious need of someone who knows how to guide me to better health using this info. Thank you for any referrals or suggestions.
Hi Dorothy, I know many practitioners who do remote / online consultations. If you are interested send me an email via [email protected]
Your article helped me understand Oxalates more clearly. Some sources say that PEG (polyethylene glycol ) increases oxalates ,which could explain why I was in extreme pain after having a PEG prep for my colonoscopy . I had an OAT test a few days before having a colonoscopy. My OAT test came back after shortly after having the colonoscopy which showed my oxalates were very high along with yeast markers. I am scheduled to get my Pfizer vaccine ,which has PEG in it . I am wondering if anyone knows if having PEG injected intramuscularly will increase oxalates or is it just if PEG is ingested.
Hi Judy, that’s a great question. It will depend on the mechanism of action in how PEG contributes to the oxalate load. It seems that PEG may be converted to oxalic acid with the help of gut microbes. If this is the case then injected PEG may not have the same effect. PEG in vaccines may have other side-effects though as it has been associated to anaphylactic reactions in mRNA vaccines.